.1
Respiratory problems
.2
Jaundice (hyperbilirubinemia or icterus)
.3
Low birth weight (Small for Gestational Age)
.4
Short tongue tie
.5
Necrotizing enterocolitis (NEC)
.6
Oxygen deficiency at birth (Perinatal asphyxia)
.7
Patent Ductus Arteriosus (PDA)
.8
Intraventricular haemorrhage (IVH)/ Intracranial haemorrhage
.9
Crying baby
.10
Infection
.11
Congenital heart defects; ASD/VSD
.12
Congenital heart diseases
.13
Low blood sugar (hypoglycaemia)
TAKING PART IN BABY CARE
Disorders
Respiratory problems
Respiratory problems can have various causes. For instance, because of the immaturity of the lungs, an infection, meconium or fluid in the lungs as explained below. After the birth it may be that your baby has difficulty breathing.
SYMPTOMS

Diagnosis
When there are breathing problems, the doctor can decide to take some blood. The gas exchange in the blood and the infection levels are checked. Apart from that the doctor can decide to have X-rays of the lungs taken.


Treatment
Your baby is connected to a monitor so that the heart rate, breathing and oxygen level in the blood can be monitored. Often it is also necessary to support the breathing, for instance with CPAP or High Flow. The recovery depends on the seriousness of the symptoms. In the case of a wet lung for instance, the fluid in the lungs is often absorbed by the body within a few hours. Your baby will probably get better quickly. In breathing problems because of immature lungs, this recovery may take a few days because the body needs time to produce surfactant. Often breathing support is needed, for instance with CPAP or High Flow. This is also often needed when there are breathing problems because of an infection or by the meconium aspiration syndrome. If more support is needed, your child can be given mechanical ventilation or even more complex treatments to support the lungs and the heart function, and your child will receive pain relief.
Disorders
1 Immature lungs
A newborn baby born before the 37th week of pregnancy (premature) has immature lungs. In This pathology is called “hyaline membrane disease”. The younger the prematurity is, the more immature the lungs are. In addition, it may be that there is not yet enough of an important substance for the lungs (surfactant, see also the Glossary). In the event of an imminent preterm birth before the 34th week of pregnancy, the mother will receive corticosteroid (celestone) injections that makes sure that the surfactant in the baby is produced faster. Within 48 hours after the first injection the lungs will have developed so far that after the birth the breathing problems do not occur or to a lesser extent. However, some premature babies, especially those born before 32 weeks’ gestation, may require administration of surfactant after birth. This surfactant is administered directly into the trachea. This pathology is called “hyaline membrane disease”.
2 Wet lung
In utero, foetal lungs are filled by amniotic fluid which is squeezed out at delivery when alveoli are opened and filled in with air with the establishment of first breaths However, some babies have difficulty getting rid of the amniotic fluid that is left in the lungs. We call this “wet lung”. If it takes too long before the amniotic fluid is completely cleared from the lungs. A couple of factors that increase the risk of getting wet lung are a caesarean and a fast delivery. If your baby has breathing problems, it can be necessary to support your baby’s breathing. Usually, the High flow or CPAP will be used. For more information about this, look at ‘respiratory support’. In general, wet lung recovers quickly, usually even within 24 hours
3 Meconium-containing amniotic fluid and meconium aspiration syndrome
Meconium is the first defecation of a newborn baby and is green/black and sticky. Sometimes your baby already defecates in the amniotic fluid because of stress before or during birth. This is called meconium-containing amniotic fluid. Your baby may inhale this before or during the birth. This meconium can enter the lungs. This can cause respiratory problems after birth. We call this the meconium aspiration syndrome, ie MAS. In the case of MAS, there may be an added infection of the lungs (pneumonia) so antibiotics will be administered. The infection will be monitored through blood analysis.
In about 10% to 15% of the births we see meconium in the amniotic fluid. It usually occurs in babies who are born on time or late (late is after 42 weeks of pregnancy). In a longer pregnancy, the hance of meconium-containing amniotic fluid increases.
4 Pneumothorax
If an alveolus breaks, air gets between the lung and the chest wall and consequently, the lung is collapsed. This causes a decrease in the lung´s total volume, depending on the amount of air which is coming out the lung and the baby may develop serious breathing and even circulatory problems. If your baby shows symptoms, then a tube will be placed into the chest cavity in order to release the air that has leaked into the chest cavity.
Jaundice (hyperbilirubinemia or icterus)
After birth, every baby turns yellow and this is a normal process. This is because your baby has many red blood cells that are destroyed in the first couple of days after birth. This breakdown of these red blood cells causes bilirubin to be released. The bilirubin is then built up in the blood and skin, which causes the skin to turn yellow. Bilirubin is naturally converted in the liver and excreted via the urine and faeces. Sometimes, babies need help getting rid of the excess bilirubin levels in their body, and this is done via phototherapy. It is important to monitor the bilirubin levels of newborn babies because if they are too high, it is toxic to the brain.
In babies born before the 37th week of pregnancy (premature), the organs are still immature and is therefore common for premature babies to need treatment for jaundice. Sometimes there is an incompatibility between the mother’s and the baby’s blood, causing a greater destruction of red blood cells that worsen hyperbilirubinemia. Also, excessive weight loss can cause hyperbilirubinemia.
Yellow colouring of the skin and the whites of the eyes. Drowsiness and less alert. Drinking less well.
The degree of discolouration of the skin does not say anything about the height of the bilirubin level in the blood. The nurse will observe your baby’s yellow skin colour. In a premature baby, it is standard to check the bilirubin level in the blood several times within the first few days.
If it has been established that the bilirubin level in your baby is too high, phototherapy will be initiated. This is a blue shining lamp or LED lamp that makes sure that the waste material bilirubin is broken down. Your baby will be placed naked with only a nappy on in an incubator or on a heated bed so that they remains at the right temperature, and so that as much of their body is in contact with the phototherapy light as much as possible. As a result of the phototherapy, your baby’s faeces will often become softer and the colour of the urine will become darker. While your baby is under the light, their eyes will be protected by cloth glasses. When phototherapy is given, it is important that your baby receives enough fluid. Sometimes it may be necessary to give extra fluids via an intravenous drip. If the bilirubin level in the blood is extremely high, it can damage the brain. That is why it is important for your baby to stay under the phototherapy lamps for as long as possible and it may mean that skin-to-skin care is not possible.
For more information about phototherapy, also see the article on “Phototherapy lamps”.
Low birth weight (Small for Gestational Age)
A SGA baby has a lower birth weight than might be expected for a gestational age. For this the abbreviation SGA is used, meaning ‘small for gestational age’.
CHARACTERISTICS
The head is relatively large compared to the body. The face often gives the impression of being older. Subcutaneous fat is lacking, the skin folds are large and the skin is dry. The newborn baby appears alert and hungry.
Special care for the SGA baby
To a large extent the care for a SGA baby is the same as the care for a premature baby. The degree of dysmaturity mainly determines which special care your child needs.
We pay extra attention to the following points:

Short tongue tie
Sometimes a baby has a tongue tie that is too short. A short tongue tie is when the tongue tie is very tight or short or if it is attached almost to the tip of the tongue. This limits the tongue´s movements. A short tongue tie can make it harder for your baby to latch on well for breastfeeding or to get a good grip on a breast. A short tongue tie can be recognized by the heart shape form of the tongue. But sometimes the short tongue tie is only noticed because the baby cannot stick his tongue out properly. It is not always necessary to cut the tongue tie if your baby is not bothered by the short tongue tie, and, for instance, drinks well from the breast.

Oxygen deficiency at birth (Perinatal Asphyxia)
Oxygen deficiency, or asphyxia, can take place during pregnancy or around the delivery. If the oxygen deficiency occurs around the delivery, it is called perinatal asphyxia. If oxygen deficiency has occurred, this can be damaging for various organs, like the brain and the kidneys. If the brain is affected, the clinical state secondary to oxygen deficiency is called hypoxic-ischemic encephalopathy (HIE). The damage to the organs and intensity of HIE is dependent on how long the oxygen deficiency lasted and how deep the oxygen deprivation was. It’s true extent is hard to predict when the baby is very young.
At birth the Apgar-score is done by a doctor or a nurse. This is a test that assesses your child’s condition after birth. The score goes from 0 to 10; the best score is 10. In addition, blood will be taken. Among other things, the acidity level in the blood will be checked. If there is too little oxygen in the blood, then the blood will become acid. The greater the oxygen deficiency is, the more acidic the blood will become. If HIE is suspected, it is necessary to carry out an ultrasound of the brain, electroencephalography monitoring and neurologic evaluation.


In the event of oxygen deficiency the treatment is aimed at supporting the body functions, like breathing, the heart rate and the oxygen level. In addition, your baby will have minimal handling. That means that we let your baby be as much as possible and try to combine activities. It can also be the case that extra fluid is given and possibly medication, like antibiotics. If HIE is suspected the brain activity will be recorded and possibly a special cooling therapy will be started. This treatment entails cooling the baby to a temperature of 33 °C for 72 hours. The cooling means that the baby’s body needs less energy and less oxygen. In this way any damage that may occur in the brain because of oxygen deficiency can be limited. Children are cooled with a special cooling package that keeps the baby’s temperature precisely within the right limits. In addition, your child will be given medicine to make sure that he/she stays comfortable. After three days he/she will slowly be warmed up to the normal body temperature of 37°C.
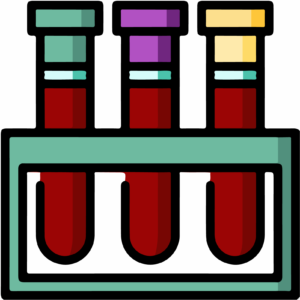
Patent Ductus Arteriosus (PDA)
The ductus arteriosus (or: ductus Botalli) is a blood vessel that connects the pulmonary artery to the main artery in the body (aorta). This blood vessel has to stay open during pregnancy (patent) so that oxygenated blood from the placenta can reach the aorta and the rest of the body via the pulmonary artery. But after birth this blood vessel has to close. This actually always goes well in babies born full term. In premature babies it is possible that this blood vessel does not close immediately and closes later. The blood vessel stays open for a prolonged period. This is mainly seen in babies born before 30 weeks of pregnancy.
If the blood vessel does not close after birth, it can cause problems (mainly breathing problems). Sometimes there are small signs that your baby still has an open ductus, namely that the blood pressure is low or a murmur is heard when your baby is examined.
A heart ultrasound needs to be done in order to show that this blood vessel is still open in your child. Depending on how much of a problem it is for your baby and what the size of the ductus still is, treatment may be started. It is also possible to choose to just wait and see.
The treatment usually consists of giving ibuprofen via an intravenous drip for a few days. It is possible to choose to give less fluid and some extra diuretics. It is not always possible to close the ductus (completely) with ibuprofen. In some cases, it will be decided to close the ductus by cardiac catheterization or an operation.
Intraventricular haemorrhage (IVH) / Intracranial Haemorrhage
Intraventricular haemorrhage is a bleeding in the ventricles of the brain. The ventricles are filled by a fluid, the cerebro-spinal fluid (CSF), that is produced and reaobsorbed continously. This is an important complication in prematurely born babies, and mainly occurs in babies with a birth weight under 1500 grams. This bleeding usually occurs in the first days after the birth. After this, the chances become much smaller. If IVH is large enough it may become complicated by progressive growth of the ventricles due to obstruction of CSF circulation, causing post-hemorrhagic hydrocephalus. Another frequent site of bleeding in the preterm infant is the cerebellum.
The blood vessels are still vulnerable in this group of children, and, with any fluctuations in the blood pressure, a haemorrhage in the network of undeveloped blood vessels may occur.
Usually in premature children there are no clear symptoms. Sometimes epileptic seizures can occur. But also:
An ultrasound of the brain will be done regularly in the first week in order to monitor and check the brain. Most haemorrhages have no or hardly any consequences, but sometimes a venous infarct ion surrounding the ventricles can occur. These complications may have a significant impact on your baby’s outcome. If a haemorrhage is discovered, ultrasounds will regularly be done to see if there i any associated complication. Sometimes a MRI scan is also done to gain more clarity about the location of the bleeding and the possible long-term consequences.

There is no treatment for an intracranial haemorrhage. We only treat associated factors, such as anemia. If hydrocephalus develops, it can be treated by removing CSF at variable intervals, either by lumbar puncture or using devices that are inserted into the ventricular space.
If a brain haemorrhage is discovered in a child, it is a worrying time for the parents. There are often many uncertainties about how it will go and what the developmental consequences will be.
It often happens that a baby has no long-lasting consequences from an intracranial haemorrhage. Of course, that is the best possible result parents can hope for after a period of uncertainty. But it can also happen that a baby does have some longterm sequelae. The consequences can differ greatly, depending where the haemorrhage was located and what is damaged. In some cases the motor development can be delayed. By starting early on with guidance from a physiotherapist, these consequences can hopefully be limited. An MRI on the due date can often offer more clarity about the long-term consequences.
Crying baby
All babies cry, that goes with the young age. It is a way to communicate with you as a parent. A baby cries when he/she is hungry, has a dirty nappy, wants some attention, is in pain, does not feel well, is stressed, or is just tired. Everywhere in the world we see that babies increase their crying from birth to the age of 6-8 weeks. At that age babies cry for on average 2 to 2.5 hours per day. After that, the number of hours babies cry usually decreases. From the age of 12 weeks on, the number of hours of crying stays between 1 and 1.5 hours a day for the rest of the first year of life. Usually the crying can be interrupted and your baby can be comforted by contact, attention, care and feeding. Sometimes a baby is really inconsolable. In less than 5% of all babies who cry inconsolably, there is a physical cause for the crying.

Examples are:
So, in the remaining 95%, there is no obvious physical cause found. Often there are baby and/or parental factors and especially the interplay of those factors.
This can be things like:
Actually, this can be anything that makes reacting to the baby’s signs more difficult, like:
If there are both baby and/or parental factors, the relationship between parents and the baby can be put under pressure. Your baby’s crying can increase and your baby (and often the whole family) become more and more upset. Apart from an increase in crying, your baby may also develop feeding and sleeping problems. Finally, a vicious circle is created that is hard to break. If you think your child is in pain, cries unusually often or loudly or if the crying worries you, call your GP or the child health clinic.
Kangaroo care and carrying your baby are good ways to co-regulate your baby, calming the stress system down. See in the library for kangaroo care, carrying your baby, developmental care, caring together and FICare. What can you do if you yourself become anxious or upset by your baby’s crying? Make sure your baby is in a safe place, for instance, in the cot or the playpen. Sit in another room for a short while to calm down. It is better not to pick your baby up if you are irritated. Go back to your baby when you feel calmer. If you notice you cannot handle your baby’s crying any longer, ask your family or friends for help. Do not wait until you are totally desperate. Your baby might even hold his breath while crying because of strong emotions. Your baby may even turn blue because of it. Try not to panic, put your baby on his side and tickle the soles of his feet. Your baby will then usually breathe normally again. Blowing softly into his face can help too.
Do not shake your baby. That is actually very dangerous. A baby’s head is big and heavy compared to the rest of the body. Without support the head will fall backwards. The muscles in the neck are not yet strong enough to hold the head up. If you shake your baby, the small veins in the brain can burst and cause bleeding. This can have serious consequences. If you witness your baby being shaken, it is important to go directly to the nearest hospital’s Emergency Department. Even if you are the person who shook your baby. Fast help may prevent serious damage.
Make sure your baby is in a safe place, for example, in the cot or playpen. Sit down for a while to try to calm down – it is best not to hold your baby if you are nervous. Come back to your baby when you feel better. If you find you can no longer cope with your baby’s crying, ask family or friends for help. Don’t wait until you are totally desperate.
When a baby cries a lot, there may be brief moments when they do not breathe (colloquially ‘deprived’) or even change the colour of their skin (cyanosis). If this happens, try to stay calm, turn your baby on their side and tickle the soles of their feet or gently blow on their face. They will usually start breathing again after this. Never shake your baby, it is very dangerous. A baby’s head is large and heavy compared to the rest of the body. Without support, the head will fall backwards as the neck muscles are not yet strong enough to support it. If you shake the baby, the small veins in the brain can rupture and cause bleeding that can have serious consequences. If you see your baby being shaken or you have shaken your baby yourself, consult your paediatrician or go to the Emergency Department so that your baby can be examined.
Infection
An infection is caused by bacteria that cause inflammation in the body. These bacteria can also be found in the bloodstream. There is then sepsis or blood poisoning.
A newborn baby’s immune system, and that of a premature baby in particular, is not yet fully developed. That is why they have a much higher risk of an infection. Premature babies also lack antibodies against specific bacteria. These antibodies are not passed on by the mother through the placenta until later in the pregnancy. Another important risk factor for an infection are bacteria that are transmitted by hands, intravenous drips and tubes. That is why it is so important to establish good hand hygiene. This goes for everybody: parents, visitors, nurses and doctors. The bacteria can penetrate various organs via the bloodstream and infect them. For instance, catheter related infection, pneumonia or a urinary tract infection can occur. One of the most serious complications of blood poisoning (sepsis) is an infection where the membranes around the brain become inflamed (meningitis).
If your baby is suspected of having an infection, blood will be taken from your baby. This can determine the level of infection in the blood. In addition, a culture is started to detect which bacteria is causing the infection. In some cases, it is necessary to do a lumbar puncture to determine if there is meningitis. During a lumbar puncture CSF fluid is taken for culture and biochemical analysis to rule out meningitis. Your baby’s urine (pee) will be collected to exclude a urinary tract infection. This urine will also be cultured. In addition, a lung X-ray can be taken in the case of breathing problems.

Antibiotics will be started as soon as the tests have been done. Because the culture results take at least 2 days, we will start with antibiotics that fight many bacteria. The antibiotics will be administered via an intravenous drip.
When the test results show that an infection is unlikely, the antibiotics will be stopped. If bacteria are found, the duration of the antibiotic treatment depends on which bacteria is found and where it is. The duration of the treatment in a proven sepsis, for example, is 7 to 14 days. If meningitis is diagnosed, then the duration of the treatment with antibiotics is 2 to 3 weeks.
Each infection is different. The majority of babies recover within a few days after starting antibiotics. If your child recovers well from the infection, then in most cases there are no serious consequences for the baby’s development. This is indeed dependent on the seriousness of the infection and if there had actually been meningitis. In some cases, it is not an infection with bacteria but an infection caused by a virus. This is called a viral infection. A viral infection cannot be treated with antibiotics. In the majority of cases the body will have to fight this infection by itself.
Congenital heart defects
A congenital heart defects are a malformation of the heart or large blood vessels that occurs in the development during pregnancy. There are many types of congenital heart defects, depending on which structure is affected.
Most congenital heart defect are diagnosed during pregnancy, but some are diagnosed after the birth of the baby due to the presence of:
We can suspect a congenital heart defect based on the symptoms above. To confirm we will perform a cardiac ultrasound (echocardiography).

Some congenital heart defects are mild and only require periodic cardiological check-up, with or without specific treatments. Others are life threatening and require surgery in the first days of life due to their greater severity, and will even require other surgeries or cardiac catheterizations throughout their lives.
Usually a complete correction can be achieved, reaching structural and functional normality of the heart. In some cases, there is no surgery repair but this surgery could be be palliative to try to make the baby’s quality of life as good as possible. In many cases, the baby will need to take medication for a long time to facilitate the correct functioning of the heart and thus improve its quality of life.In either case, the condition of having heart disease is permanent. The babies who are born with this type of structural alterations of the heart must undergo medical and specialised monitoring throughout their lives.
Pulmonary hypertension
Pulmonary Hypertension (PH) occurs when the lung blood vessels may not open up properly or the pressure inside them remains high. As a result blood cannot get into the lungs to pick up oxygen and then the body will not have enough oxygen for the brain and other organs, and this can make a baby unwell. The heart needs to work harder to carry the blood to the lungs.
We will suspect the presence of PH because the newborn has a low oxygen saturation which requires supplemental oxygen that may be accompanied by respiratory distress or cyanosis. The course is variable in each baby. But the presentation can be severe, putting his life at risk.
A cardiac ultrasound can be performed to measure the pressure in the heart. In very rare cases a cardiac catheterization is needed.
The administration of oxygen is the main treatment. It will dilate the pulmonary artery so the pressure decreases and causes a better functioning of the heart. Other measures that may be needed to treat PH are the use of sedation to make the baby calmer; medication to improve heart function and dilating the pulmonary artery.
Low blood sugar (hypoglycaemia)
Glucose (sugar) is an important source of energy for all body processes, especially for the brain. During pregnancy your baby will receive glucose via the umbilical cord. In the last phase of pregnancy a reserve is stored. The doctor will decide if your baby’s blood sugar has to be checked after birth. If your baby cannot regulate his blood sugar level, and because of that has an insufficient glucose level in the blood, this is called low blood sugar or; hypoglycaemia.
The sugar level is not checked as standard after the birth of every newly born baby. Standard checks are only arranged for babies who have an increased risk of having low blood sugar.
A low glucose level does not always cause symptoms. If that is the case, those symptoms can be the following:
If your baby is in a risk group and after a consultation with the doctor, a drop of blood will be taken from the heel at different times. The amount of sugar will be established from this drop of blood. This is to detect and treat a low sugar level. In principle, the sugar level is determined at different moments in the first 24 hours. If the sugar level is still not right, extra checks will be added on.
The treatment depends on the sugar levels (glucose). At first the aim is to maintain the blood sugar level at the right level through feeding. If this does not work or if your child does not manage feeding, then your child will get an intravenous drip so as to be able to have a continuous supply of sugar. As soon as the sugar level has recovered, we reduce the amount of glucose that your baby receives via the intravenous drip and we increase the feed until the intravenous drip can be stopped completely. During this process blood will be taken several times in order to measure the sugar in the blood.