.1
Breastfeeding: general information and advice
.2
Giving breastfeeding and problems
.3
Breastfeeding with bottle
.4
Expressing & keeping breastmilk
.5
Formula feeding
.6
Learning how to drink
.7
Conditions for drinking
.8
Hunger signals
.9
Regulating the ‘flow’ with the bottle
.10
Positioning during feeding
.11
Non-nutritive sucking
.12
Tube feeding
.13
Parental nutrition
.14
Balance
.15
Orofacial sensori-motor stimulation (OSMS)
.16
Orofacial stimulation guidelines
.17
Pacifier
TAKING PART IN BABY CARE
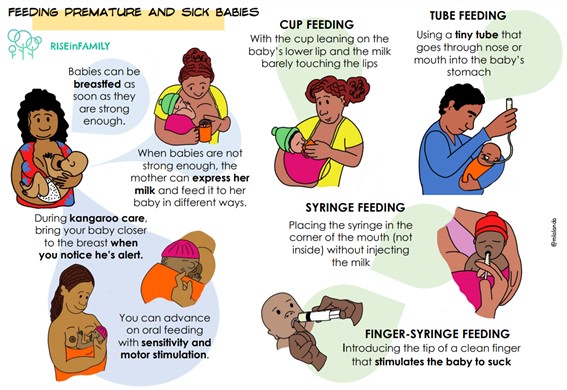
Feeding the baby
Breastfeeding and general information
During your stay in hospital, you will be expertly guided to make breastfeeding a success. Breast milk is recommended as the first choice for feeding your baby. However, whatever you choose, breastfeeding, formula feeding or mixed feeding, every choice is good.
Advantages of breastmilk for your baby:

For your baby there are no disadvantages from breastfeeding.
Advantages of breastfeeding for the mother:

Some disadvantages for a mother can be:

Breastfeeding: general advice

Breastfeeding should be a pleasant and special experience for mother and child. Below is some advice.
Advice on food and drink: If you breastfeed, you use extra energy. That is why it is important that you eat a healthy and varied diet. You can eat and drink everything, but be aware of how your baby responds to it. Some products you eat can irritate your baby’s digestive system. Which products these are varies strongly from baby to baby. It is best to give it a try. Drink enough (at least 2 litres a day). What works well is drinking something yourself every time you breastfeed. If you drink too little, you will notice that your mouth becomes drier than usual, you will be thirsty and yoururine will also be a darker colour.
Your baby can become restless from drinks containing caffeine, if drunk excessively. Be careful with alcohol. It is not recommended because alcohol goes quickly into the breastmilk.

Giving breastfeeding
If the circumstances allow it, it is so nice to have your baby skin-to-skin after the birth, and recover together. Many babies will only cry for a short time and rest for a little while and then start searching for the breast. In the first hour after birth the baby will be quiet and alert, the sucking reflex is then at its strongest. If pain medication was given during the delivery, it may take a little longer before the baby is alert enough. The paediatrician will decide on how long your baby will stay in the delivery room, depending on your baby’s state.

Points of attention for breastfeeding:

The ideal way of feeding is feeding on demand. But in many premature or ill newly born babies this is not feasible in the beginning. The nurse will help you with breastfeeding every day. For questions in some hospitals, you can contact a lactation consultant or a preverbal speech therapist. If your baby is with you in the room, you can react to his need for physical contact and feeding. You feed your baby when you notice that he is ready for it. You can feed your child for as long as he/she drinks effectively, that is drinking regularly with long gulps. If your baby starts sucking, take him/her off the breast and offer the other breast. Your baby needs a minimum of 8 feeds every 24 hours. On average your baby will drink from the breast 8-12 times a day. You can offer both breasts each time. This helps start the milk production. Each time first offer the breast which you stopped with at the previous feed and then offer the second breast. It may be that the baby is already satisfied after the first breast and does not want the second breast. That is fine too. By often latching the baby on, you stimulate the milk production sufficiently. Some babies do not suck well on the breast the first few times. He/she will often only lick or fuss with the nipple. You do not have to worry about this as this also stimulates breastfeeding. Some babies are a bit sleepy or slow in the first few days. In the first 24 hours this sleepiness is very normal.
See also the article “Learning how to drink”.
Breastfeeding with bottle
If your baby has been admitted to the department of neonatology and you cannot latch your baby on yet, it is still possible to breastfeed.
Supplementary food
While you cannot breastfeed, it is important to trigger the breastmilk by expressing. The expressed milk can be given by bottle, finger feeding, cup or nasogastric tube, depending on the department’s policy. It is important to offer your baby the breast regularly, as soon as the situation allows. If your baby is in hospital, it is possible that the paediatrician has specified that your baby needs supplementary food. Supplementary food is all the nutrition your baby receives other than breastfeeding. This is prescribed when the baby cannot drink enough from the breast. Supplementary food is preferably your expressed breastmilk, possibly supplemented with formula feeding.

Expressing
If your child gets supplementary feeding, it is important that you start expressing in addition to latching the baby on. We advise you in this case to express milk in order to make your breasts produce enough milk. In some departments a breastfeeding help set is used, ask the nurse for information about this. The baby will receive the supplementary feeding through a thin tube in the corner of his/her mouth while being breastfed. Ask the nurse about this option.
Own bottle and teat
Before you are discharged, we advise you to start using your own bottle and teat. This can be done in consultation with the preverbal speech therapist or nurse. For premature babies we advise starting with a premature teat, so that the baby does not choke so easily.
Expressing & keeping breastmilk
Expressing
If everything goes well and your baby is feeding well at the breast, a pump is not necessary. However, there can be reasons why breastmilk needs to be expressed. Reasons can be:

Consult a care professional if you need to start expressing milk. When you are separated from your baby, it is important to start expressing as soon as possible. If it is possible in the first 2 hours after birth. Ask for help if you are staying in the hospital. Every situation requires a different expression schedule and sometimes also a different pump. There is a lot of information on expressing breastmilk.
Keeping breastmilk
Write down your baby’s first and last name on stickers, along with the date and time of expressing and any possible medication you have taken, and stick these to the bottles. Put the expressed milk in the refrigerator straightaway or give this to the nurse. Breastmilk may be kept in the refrigerator for 48 hours. If there is extra milk, it can be frozen. The milk must be put in the freezer within 24 hours and can be kept for 3 months. After thawing the milk must be used within 24 hours. Other rules apply at home.
Formula feeding
After careful thinking, you can make your own choice whether to give your baby breast or formula food. Before you make the choice, it is good to have information on this important choice. How shall I feed my child? If because of certain circumstances you cannot or do not want to give breastfeeding, formula food is an alternative. You can expect professional help for both breastfeeding and formula feeding in the department. Special premature nutrition is given depending on your baby’s age and weight and otherwise standard infant formula feeding is used. In the department disposable bottles and teats are used in the first period of the hospital stay. Of course, you can use your own bottle. Depending on your baby’s age and drinking technique, a bottle with a narrow teat may be sometimes recommended in consultation with a speech therapist and nurse. Before buying a bottle, ask them for advice. After being discharged, you may switch to another formula unless the doctor has prescribed special nutrition. Before you go home, talk to the nurse about how to prepare formula for feeding at home. See also the article “Tips for at home”.
Learning how to drink
Good coordination is important for the baby to be able to drink well and safely from the breast or the bottle. When it is time to start feeding via the mouth, you can choose the breast, bottle or a combination of both. In the first few months your child will drink reflexively. This means that your baby turns his/her head towards the breast or bottle when he/she is hungry and when the breast or bottle touches the mouth. The sucking starts when the nipple or teat enters his/her mouth. If you want to breastfeed, start practising with the breast first and then the bottle. If your child does not have enough energy to drink all he/she needs from the breast, but is able to drink from the bottle, then often a combination of breastfeeding and expressed milk using the bottle can be given. If breastfeeding is not possible, formula feeding or sometimes donor milk is given in some institutions. Ask your doctor about this.
As a parent you will learn from the nurse, lactation consultant or the preverbal speech therapist (if available) how you can help your baby to learn how to drink. The preverbal speech therapist specialises in swallowing, eating and drinking problems in very young children.
The ideal would be breastfeeding on demand, trying to feed in response to the baby’s demands. However, in hospitalized babies without autonomy for oral feeding, we maintain a fixed feeding schedule, every three hours as a general rule. There are babies who need to feed every two hours. In some cases, in children who are already breastfeeding, taking a demand or semi-demand can be evaluated.
Conditions for oral drinking

Feeding short but right
In the beginning your child will become tired fast and may not drink for too long. If your child is well awake and if he/she shows signs of wanting to feed, then it is a good moment to practise drinking. When your child is relaxed and sufficiently alert to start drinking, his/her fists will be slightly clenched. It is important that he can maintain sufficient muscle tension. If your baby holds his/her hand out (stop sign), then your child is asking for a break. If the arms and legs hang loosely down by the body, there is too little muscle tension to drink properly. Your child is tired and cannot drink any longer.
It is more important that your child feels at ease at feeding times than how long the (breast) feeding lasts or how much he/she drinks. What helps is a quiet place with pleasant light and a shawl to keep your child at the right temperature. How long a child is willing or able to drink depends on his/her age and health, but generally it will not last longer than 30 minutes.
Hunger signals
A baby is ready to feed if he/she shows teat or nipple seeking reflexes. You can recognize this by gently stroking his cheek towards his mouth or stroking his/her lips. Wait at the middle of his/her mouth for his/her response. Your baby will open his/her mouth and suck on the nipple, or teat him/herself. It is important to let your child react to this reflex by him/herself. In this way the baby learns that a nipple or teat is not just randomly put in his/her mouth, but that this is the result of his/her own reaction.
The nurse, lactation consultant and/or preverbal speech therapist will help you to recognize your child’s hunger signals. Similarly, during and after drinking your child will give signs as to how he/her feels and about drinking. By looking at those signs together you will learn how you can best help your child to drink. Enough time between the feeding is needed to make sure that a child really feels a little hungry and to recover from the effort of drinking.

Regulating the ‘flow’ with the bottle

Never force your child to drink, but let him/her indicate when and how much he wants to drink him/herself. It is important that your child can manage the amount of milk (flow) that comes from the breast or bottle. It can help to reduce the extra pressure in your breast by expressing before you start feeding. By adjusting the shape of your breast with your hand (C or U grip) your child can more easily latch on. Sometimes a nipple shield can help your child to get the breast properly in his/her mouth.
Bottle advice: If you give bottle feeding, you can choose from various sorts and sizes of teats. If your child still has difficulty with the coordination of breathing, sucking and swallowing, then there should not be too much feed coming out of the teat in one go. You need a teat that gives less flow: a ‘low flow’ or a teat, especially for premature babies. The nurse, lactation consultant and/or preverbal speech therapist can help you make the right choice.
Positioning during feeding
Feeding can be done in different positions. It is important that your child’s neck and back are kept in a straight line. That makes drinking easier and your child will be able to drink better with good coordination. Sometimes it is necessary to adjust the position as it will improve the baby’s ability to drink. Premature children are often fed on their side. This position imitates that of breastfeeding and allows them to drink comfortably and for longer. The side position is often no longer or only needed for a short time once your baby is at home. Together with a nurse and/or preverbal speech therapist or lactation consultant look for the position that works best for you: on his back, on his side, slightly supported by swaddling and/or the use of a (nursing) pillow. It is always nice to keep visual contact with your baby.

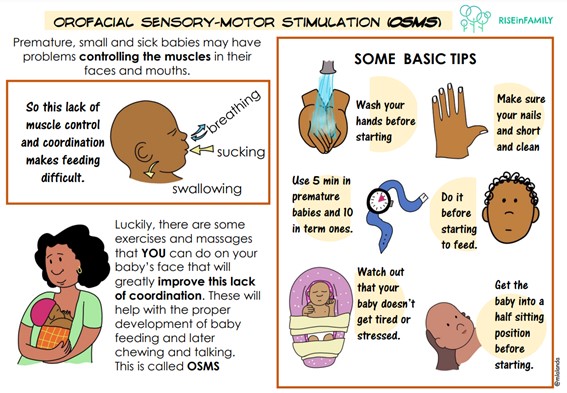
Orofacial sensorimotor stimulation (OSMO)
Orofacial sensory-motor stimulation (OSMO) is the concept of improving the function of the muscles of the face and mouth to achieve an adequate functional suction-swallowing process with good coordination of breathing and swallowing. This is achieved by exercises and massages.
The feeding function
The orofacial system is responsible for the functions of breathing, sucking, swallowing, speech and phonation. The progression of oral feeding has several phases:
During sucking, each oral structure plays a specific role that ensures proper function:

Sensory-motor-oral functional alteration
If your baby has motor problems in the face and mouth, he/she will use the available sensory and motor responses which can result in abnormal movement patterns.
Symptoms that can make us suspect an altered swallowing in a baby are:
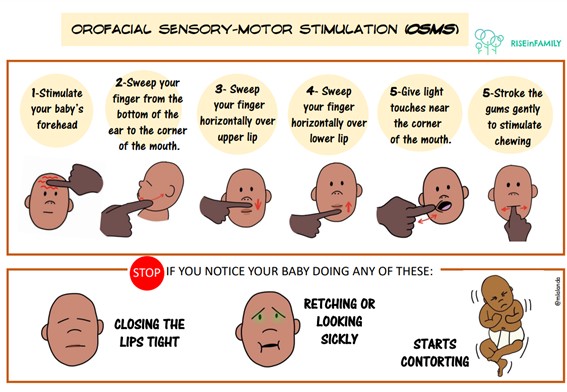
Orofacial stimulation guidelines
The perioral area is the area of the face around the mouth where very important muscles will be mobilised for the proper development of sucking and subsequent chewing. The exercises that can be performed are:
Intraoral exercises are those that are carried out inside the oral cavity of the newborn and are more invasive. These exercises help to improve the mobility of the tongue and its coordination with other structures involved in the swallowing process, such as the palate (soft palate).
Non-nutritive suction
Non-nutritive suction (NNS) is used during nasogastric tube feeding, both in preterm infants and in infants who need prior learning for any other reason. Its objective is to facilitate the development and maturation of the suckling and improve the digestion of food. NNS can be started as soon as the baby is stable, regardless of maturity. NNS precedes nutritive sucking and is characterized by bursts of sucking for short periods of time . The NNS is beneficial for the newborn, since it contributes to the physiological stability, achieving levels of oxygenation and stabilising the heartbeat while the maturation of the feeding reflexes is achieved. It also shortens the transition time from tube feeding to oral feeding.Additionally, NNS is beneficial for pain relief, self-comfort, calming the baby, regulating states of alertness and greater sleep duration. The NNS can be done on the breast, with freshly extracted milk whilst doing skin-to-skin contact. In the absence of the mother, it is recommended to gently practice NNS with a pacifier.
Tube feeding
If drinking by himself is not successful or does not work, your baby will be fed via a feeding tube. A feeding tube is a small flexible tube that is inserted through the nose or mouth by a nurse. In a baby which is born too early it will depend on his age whether or not he/she can drink by him/herself. A premature baby does not yet have a good sucking reflex. On average, you can see the following things in your baby depending on the number of weeks of pregnancy. (Remember, there are always exceptions! We will look at your child and see what he/she can handle.)
24-35 weeks: Your baby will have a tube and be fed through that tube. Your baby will also have an intravenous drip during the first period after birth for glucose and/or nutrition to be administered because the digestive system has not yet developed enough.
From 33-34 weeks the suck-swallow reflex begins, so your child can drink by him/herself but your baby does not have much energy yet. Other reasons for inserting a tube into your baby are to release air from the stomach, as breathing support and to determine retention of feeds in the stomach. Inserting a tube can be an unpleasant procedure. Once the tube is in place, your baby will not be bothered by it anymore.
When your baby indicates he wants to “drink by him/herself”, he/she will begin breast or bottle feeding. Feeding can be done by the parents or by a nurse. It is important that the whole feeding time does not last longer than 30 minutes, asit would require too much energy from the baby. Any remaining amount of milk can possibly be given via the tube.
Types of administration of milk through the tube:
It consists of the administration of milk that we load into a syringe and connect it to the tube that the child has. The rate of entry into the digestive tract depends on gravity. Only the amount of milk prescribed for each shot, previously heated to the desired temperature, will be introduced into the syringe. Next, we will unclamp the probe. The tip of the syringe should be at the level of the corner of the baby’s mouth, or a maximum of 10 cm above the stomach. It might be necessary to force the flow a bit at first.
Some newborns do not tolerate an increasing volume of milk given in a short space of time. Therefore, the solution is to slow down the rate of entry of milk into the stomach, and do it in a controlled manner at a constant rate. For this, feed infusion pumps are used, which are programmed to deliver the required amount in the desired unit of time. The procedure is as described below:
Percutaneous endoscopic gastrostomy (PEG) involves the placement of a tube into the stomach through the abdominal wall using endoscopy. It is used in patients whose oesophagus does not function for different reasons. The infusion of food through the gastrostomy tube can be done by pump or syringe.

When the syringe is empty, the tube must be cleaned with bidistilled water. After feeding the child, we will usually close the tube with the cap. If your doctor prescribes it, we will keep the catheter in the chimney, that is, hanging about 10 cm from the same plane in which the baby is lying, without the plunger, to favor the exit of air from the digestive tract.
It is difficult to predict how long your child will need tube feeding. As your baby grows older and reaches full-term age, he/she will have an increase in energy. As a result, his/her ability to drink will improve and he/she will drink more himself/herself. The tube will be needed until we see that your baby has finished drinking everything him/herself for 24-48 hours. Often a minimal amount of feeding is agreed. When your baby drinks this amount him/herself, the tube will be removed. In somehospitals even babies with tube feeding can be discharged. Consult your child’s doctor as to what the options are. Tube feeding is usually needed for a short period, but sometimes it may take a little longer.
Tube feeding care
Some parents are often uncomfortable with the presence of a tube in their baby. The collaboration of parents in the correct maintenance and use of the tube is important. You will need to regularly check the skin on your baby’s nose and face to prevent skin lesions. The area around the nose should be clean and dry. In addition, you’ll need to make sure your newborn’s mouth is cleaned regularly if he/she isn’t already feeding by mouth.
It is necessary to check the correct position of the tube (see if it is at the corresponding distance), as well as its fixation. This will minimize possible side effects from using the tube.The nurse will show you how to do that first and then you can do it together.
Parenteral nutrition
Parenteral nutrition is a method of feeding that bypasses the digestive tube. This type of feeding supplies a mixture of fluids, electrolytes, sugars, proteins, vitamins, minerals, and fats into a baby’s vein. It is indicated in any newborn in whom enteral feeding is not possible, or is inconvenient or risky, due to malformations, diseases or immaturity.
For this type of feeding, partially opaque infusion bags and tubes are used to minimize light exposure and prevent damage to their contents. A feed infusion pump is needed that allows programming of the total daily volume and the prescribed constant rate of infusion.
Pacifier
There are three sizes of pacifiers for premature babies. For further information we would like to refer you to the various sorts of pacifiers for premature babies:
The pacifier for babies up to 1250 grams. This one has the shape and size of a premature baby’s thumb. Premature babies can already suckle really well on a little pacifier. The Wee Thumbie has the shape of a small thumb and stays perfectly in the baby’s mouth.
The pacifier for babies from 1250 to 2500 grams.
The pacifier for babies from 2500 to 3500 grams.
You can always bring your own pacifier in consultation with the nurse. It is good for a premature baby to practise non nutritive sucking. In addition, sucking on a pacifier together with some sugar water (sucrose) can ease the pain and/or stress during any painful treatment. It is also a good idea to change to the right size pacifier in time in order to stimulate the jaw development. If the mother is present and wants to breastfeed, you can also use the nipple instead of the pacifier for the items above.
A pacifier needs to be boiled once every 24 hours. If a pacifier is dropped, of course this needs to be done more often.
Other feeding techniques
The choice of supplementation method depends on the circumstances and mother/father-baby preferences, with no evidence to justify one method or another: finger-syringe, syringe, bottle, cup, spoon or breastfeeder. Bottle feeding is one of the most commonly used methods but may interfere with breastfeeding, so other strategies are recommended.
The finger-syringe technique consists of inserting a clean finger into the baby’s mouth (if the technique is carried out by healthcare staff, gloves should be worn) in such a way as to make a slight lever, placing the finger in the upper part of the mouth and moving the lower jaw downwards. Never force the finger into the mouth, but rather stimulate the area so that the baby opens it. Check that the position of the lips and tongue is correct. The baby will usually start to suck on the finger in the correct position, place the tongue under the finger and suck on it, pressing upwards, with the lips well everted. Never go beyond the first third of the tongue with the finger.
Then, with the other hand, the cone of the syringe is placed on the baby’s lower lip in the space between the finger and the corner of the mouth. With the vacuum exerted by the baby’s sucking, the milk is slowly poured in, so that the baby eats while continuing to suck on the finger.
This feeding system is very fast and effective. Both hands are needed to perform the technique, so it is very difficult to do it and hold the baby at the same time. Either it is done between two people, one holding the baby and the other feeding the baby, or the baby must first be supported on an inclined surface (on cushions, a breastfeeding mattress, etc.), keeping the whole body well supported and safe. This is a good way to train sucking.
The breast pump is a container containing milk, which the mother hangs around her neck and from which, through a valve, one or two tubes or probes are attached to each breast, reaching the nipple. The tubes are small and soft and go unnoticed by the baby.
It is particularly suitable for babies who are reluctant to suckle or have a weak suckle, so that they can latch on to the breast, as with a breast pump the food flows more quickly and in greater quantity than if they were only suckling. As the baby drinks the milk from the breast pump at the same time as sucking, it stimulates the mother’s milk production and avoids problems of sucking confusion.
Balance
In premature and sick newborns, it is very important that we control all the fluids we give (for example milk or medication) and the losses they have (for example urine and stools). This helps to evaluate the well-being of your baby. You can help assess your baby’s fluid balance by weighing the diapers or checking the amount of nutrition he/she receives. The daily weight of your baby is also essential to control his/her fluid balance.

Problems with breastfeeding
It may be that problems arise with breastfeeding. It is good to know what you can do with different problems.
There are two different sorts of engorgement. Primary and secondary engorgement. Also known as physiological or pathological engorgement. Primary engorgement is a side effect of the milk production starting and is a good sign. It usually occurs around the 3rd to the 5th day. The increased activity of the mammary glands causes an increased blood supply and lymph activity in the breasts. Usually this results in light fluid retention: the breasts are harder and feel fuller and warmer. Typically, the vessels in the skin become clearly visible. The body temperature can be slightly higher. It is important to latch your baby on regularly. At least every 3 hours, but more often is also fine and normal in the first few days. Sometimes the breasts may be so tight that your baby will have difficulty getting a grip on the breast. To help with this, a little expressing by hand or a manual breast pump before the baby latches on can make it easier. Ask for help if it does not work. It is important for the whole breastfeeding period, but especially during these days, to be sure to wear close-fitting but not tight clothes. You can easily block the milk ducts in the breast with a clogged milk duct as a result.
Also known as pathologic engorgement, can have 2 causes.
For the first few days you might have trouble with sore nipples. If your baby latches on well, the nipple is protected between the tongue and the soft part at the back of the roof of the mouth. Sometimes it is a bit sore in the beginning. Normally, this pain will quickly go away. Long-lasting pain is not meant to happen with breastfeeding. Let a professional come and have a look. The cause of pain and cracked nipples is often from not latching on in the right way, causing friction in the wrong place. Skin irritation by oversensitivity to cream, nursing pads, soap or washing liquid, sensitive skin or thrush (a fungal infection in your baby’s mouth or on the mother’s nipples) can also be a cause, but does not often happen in the beginning stage. These are the causes of the problems you see at a later stage.
Latching on properly is the key to successful feeding. Ask for help from one of the health professionals if you are having trouble. In the event that you do have cracked or sore nipples, here are some tips:
You can also carry on feeding with bleeding cracked nipples. It will do your baby no harm, however, our baby might regurgitate some blood. After feeding let some breastmilk dry on the nipple (if you do not have candida). In very sore cracked nipples you may temporarily, for instance for 12 or 24 hours, switch over to only expressing instead of latching the baby on. In principle expressing does not hurt. If you do feel pain in your breast when expressing, maybe the vacuum is set too high. A high vacuum can damage the glandular tissue. If there are hard spots in your breast, they can also be sore during expressing. Always try to massage the hard areas away while expressing. You should massage towards the nipple. The temporary use of a nipple shield can also provide relief.
A sore, hard area in the breast that does not go away after a feed may indicate a blocked milk duct or a potential breast infection. A blocked milk duct occurs because the breast was not properly emptied. The remaining milk leaks out into the tissue and causes an infectious reaction or becomes thick. If this blockage is not sorted out, a breast infection may occur. Possible causes can be: the breasts are too full, for instance, by the baby not latching on right or the breasts being squeezed by an overly tight bra, sleeping on your front, exhaustion, or thrush in your baby’s mouth.
Advice for hard areas:
Too much milk sounds like a luxury problem, but it can be very troublesome for both mother and child. There can be different causes for producing too much milk (also known as hyperlactation). Ask the nurse or lactation consultant what you can do.
Advice for hard areas:
Not having enough milk is a problem many mothers experience. The causes can vary, in both mother and child. Ask the nurse or the lactation consultant what you can do.
Advice for hard areas:
Feeding skills
Breastfeeding