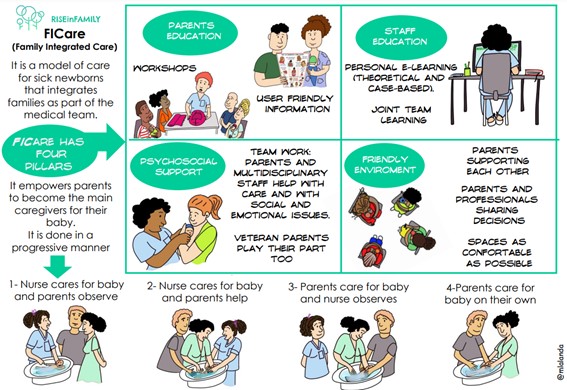
FICare model and structure of the NICU
Being a parent in the department
First contact with the NICU
Welcome to our NICU.
The news that your child has been born prematurely or with a disease can be very unsettling. This may be far from your initial expectations of your pregnancy and the delivery. Or you may have received a prenatal diagnosis and knew that your child would be born with the need of being admitted into neonatal care. Every parent experiences different emotions with their first contact with the NICU. In general, admission to the NICU for parents involves moments of anguish, uncertainty and fear. It may be that, in some cases, you react by asking many questions or, on the contrary, you do not ask any. The state of shock can lead to a block of emotions or, it can manifest with overwhelming emotions. Each person can show a different response pattern and, in this sense, the term coping refers to the set of strategies that you put into use to deal with a stressful situation. There are many different coping strategies such as active coping (e.g. problem solving) and passive coping (e.g. self-criticism). It is our team’s responsibility to contribute to the development of empowerment of your family and understand the process of adaptation and adjustment of your family to the demands of your new situation. We hope we strengthen you and your family over time.
Family Integrated Care (FICare)
Admission to the department of neonatology is a major event for parents. Many parents experience this time in hospital as an emotional rollercoaster with feelings of joy, sadness, powerlessness and uncertainty. The healthcare team’s task is to support the parents psychologically and to help them as much as possible.
Family Integrated Care (FICare) is a model of care in which parents are equal partners in the care in a neonatology department, and is often seen as an extension of the principles of Family Centred Care (FCC). FICare is originally from Canada and is used in various neonatology departments.
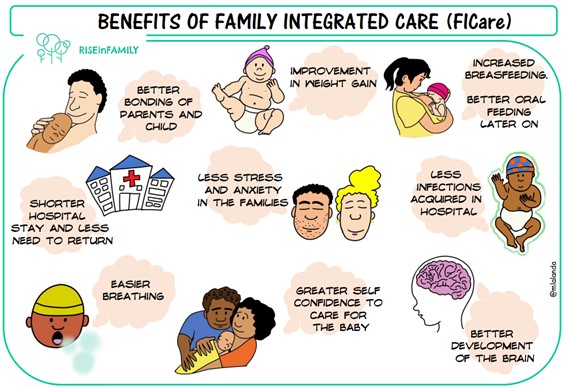
The importance of parents in the healthcare team is enormous. Research has shown that parents’ involvement in the care of their child ensures that their baby grows better. Parents’ self-confidence in the care for their baby increases, not only during their baby’s hospital stay, but also after discharge from the neonatal unit.
FICare encourages you as parents to do as much of your baby’s care as possible from the beginning. When there is a premature birth, your first reaction can often be that you feel anxious and uncertain. These thoughts are completely normal. That is why it is important that the nurses coach and support you so that you can look after your child as much as possible. We help you gain self-confidence and get to know your baby better. As your child grows stronger, it remains important that you feel you are a full member of the team in the care of your child. Your role as a parent is indispensable. Even though the nurses and doctors take care of all the medical activities, you are a unique expert in the field of your own child. Sometimes you will be the first to see if your child is doing well or not. Please do not hesitate to tell the professionals.
The FICare model consists of 4 parts that are closely related:
1. Education for parents
In order to be able to participate in your baby’s care, you need knowledge about your child’s health. The nursing staff will help you learn everything you need to know and coach you, and at the same time they will ensure good cooperation with the healthcare team. With the training, you as parents should feel confident in carrying out the care, eventually without our direct support. However, it is important to remember the neonatal team is always available to offer guidance and support whenever you need it.
Many different topics are discussed during parents’ meetings, such as support in daily care, teaching feedings and the development of a premature or sick child. Ask the nurse when these meetings will take place in your child’s neonatal unit.
2. Education for the health care team
The healthcare team must be well-trained in their role as coaches. There are special programmes available.
3. Psychosocial support for parents
Because your child’s stay in hospital can be a stressful experience for you, psychosocial support is often appreciated. This can be from a psychologist and/or social worker, but also from parents who had a child of their own in the department of neonatology. You can always get into touch with them through charities, patient associations, or at veteran parents groups in the department.
4. Patient-friendly department and culture
The setting of the department and the culture must be organised in such a way that you as a parent do not feel like a visitor, but like a real parent. As a parent, you are welcome 24 hours a day. We aim to encourage as much Kangaroo Care (otherwise known as skin-to-skin) as possible.
More information:
You will find some links here to some videos where colleagues from Canada tell about FICare (the videos are in English):
Family Centred Care (FCC)
Family Centred Care means that parents are central to giving care.The model aims to have parents involved in the care of their baby, but the nurses provide the most care for the baby. FICare is an expansion of Family Centred Care, as it results in parents being really part of the team and able to participate in their baby’s care and shared decision-making.
Family Centred Care has the following principles:
The parents work together with the healthcare team in order to make shared decisions about the treatment of their child. In this way, FCC gives the parents more self-confidence and the parents are better prepared to go home.
One of the characteristics of Family Centred Care in the department of neonatology is that the parents and child are not separated after birth (even if one of them needs extra care). Different neonatal units will offer different facilities depending on the resources available, but we should be aiming to keep families together wherever possible, with only temporary separation when medically necessary.
Family Centred Rounds (FCR)
In Family Centred Rounds (FCR), parents take part in the rounds together with the nurses and doctors. As a parent, you hear about the progress in your child’s health and you can ask questions straightaway. You can share valuable information about your baby yourself. For instance, this can include your child’s ‘general well-being’ (for example: ‘my child feels really well today’) but also medical information (for example: ‘in the past 24 hours he has had fewer incidents, his breathing is sometimes shallow, he is feeding well, or he woke up by himself to be fed’).
In order to give parents enough space to play their indispensable role during the rounds, and to participate actively in shared decisions, the nurse will explain everything beforehand so that you know what is expected of you. This will also give you an opportunity to prepare what you would like to ask and say how you think your child is doing. If you are not able to be present, there is the possibility to be present digitally and to participate in the rounds remotely. You will also grow into your role as parent by participating in the rounds. The aim for the rounds is to have protected time for you to have your questions answered, so that you know what is happening with your baby and also how you can help them in their neonatal journey. The difference between these rounds and regular medical rounds is that it is you as parents leading the round, telling us about your baby. It is also aimed to include other members of the multidisciplinary team when possible, to offer true holistic care. If you are interested then please ask the team for information about this.
Also look at the article “Rounds”.
Map of FICare training for parents
This chapter provides a map of FICare training for parents. The activities that you will be able to carry out will depend on the weeks of gestation and the maturity of your baby, their disease status, and the progress of the learning to participate in the care of your baby. The maps are organised in weeks of gestation. The nurses maintain their responsibility in standard care but they will also help you in your role as the primary caregiver. This requires building a relationship of cooperation and trust between the nurse and you.

POST-MENSTRUAL AGe less than 26 weeks
If the conditions of your baby allows it, we encourage attachment by initiating skin-to-skin contact in kangaroo care. Identify the state of your baby: are they awake and responsive or are they asleep? If they are asleep, providing comfort measures to prepare them will help. This might include controlling the intensity of light, noise and humidity; doing some comfort holding; and talking with your baby. Tremor movements, sneezing and changes in their breathing pattern could be a sign your baby is feeling overwhelmed: slowing down the pace and doing those comfort measures will help. The nurse will help you with these observations.

POST-MENSTRUAL AGE between 27 and 30 weeks
If the condition of your baby allows it, we encourage attachment by initiating skin-to-skin contact in kangaroo care, as well as other sensory stimulation procedures (parent-infant eye contact). Identify the state of your baby: are they in an awake state or are they asleep, and if they are asleep, what stage of sleep are they in.
POST-MENSTRUAL age between 31 and 35 weeks
If the condition of your child allows it, we encourage attachment by initiating skin-to-skin contact in kangaroo care. Identify the state of your baby: is he in an awake state or is heh asleep, and if he is asleep, what stage of sleep is he in. If he is in an active state, we can take advantage by interacting with him.
Caring together
We try to involve you as soon as possible in the care for your baby. You can read more in the articles “Family Integrated Care (FICare)” and “Developmental Care”. It is normal that you might be anxious, especially if your baby is still small. We will begin step by step and you can indicate what you do or do not like. You can always hold your baby during the care, certainly premature babies really like this.
We try to care for an ill or premature baby with 2 persons, preferable with the parents. This does not always happen. One person cares for the baby, the second person holds the baby. Hold with a flat hand. Try to position the baby curled up, so that the baby’s hands can be held near the mouth. Dim the light, if possible, or shield his/her eyes from the bright light with a hand or a cloth. If the baby seems stressed, try stopping what you are doing, if possible, and confine your baby with your hands. Always try to stay in contact with your baby and do not let go unexpectedly. It is useful to get everything you need ready before caring for the baby.
Always try to do this before a feed so as to disturb your baby’s sleep-wake rhythm as little as possible.

Integrated Family Care
Familly Centered Rounds