.1
Medical equipment
.2
Incubators, heated beds and cots
.3
Monitor
.4
Light and noise
.5
Breathing support
.6
Suction Equipment
.7
Intravenous drips
.8
Phototherapy lamp
.9
Bladder catheter
.10
Stoma
.11
Treatment of wounds
.12
Inhalation medication
TAKING PART IN BABY CARE
Equipment and special treatment
Medical equipment
You will see a lot of equipment around your baby which is necessary to monitor and treat your baby. Only the nurses and doctors may use this equipment. They know whether an alarm is “false” or if action must be taken. Once the nurse, who determines if your baby is stable enough, has given you consent and explained it all, then you may be allowed to connect and disconnect the wires to/from the monitor yourself. For instance, when your child has a bath or is weighed before and after breastfeeding. You should not touch or use the other equipment, such as intravenous pumps and respiratory equipment.

Incubators, heated beds and cots
An incubator, heated bed or cot will be chosen according to your child’s weight and condition. You can find out more about why your baby may need help with maintaining their temperature in the chapter ‘Characteristics of a premature baby’.

Monitor
The monitor checks various important body functions like breathing, heart rate, blood pressure and the amount of oxygen (saturation) in the blood. Should the values go outside the set alarm limits, then a signal will go off. When your baby moves, it is possible that the monitor may not measure correctly and cause the alarm to ring. This does not always indicate that something is wrong. In some units there is also a screen displaying the measurements at the nurses’ desk to alert them and the nurses have the opportunity to look at it in various other places too.


Light and noise

Breathing support
There are different ways to help your baby with breathing. You can find more information in chapter ‘Respiratory problems’ about why your baby may need help with their breathing.
Low flow means that your baby will get a small amount of warmed-humidified air blown into their nose via nasal prongs.
If your baby needs more support than the low flow, more pressure can be given through high flow to help keep their lungs open. High flow is warm and humidified air that is blown into the nose by means of a nasal mask.
CPAP is able to give more support to your baby, by giving them more pressure than high flow, to help keep their lungs open. CPAP stands for Continuous Positive Airway Pressure. By blowing air in through your baby’s nose, pressure is applied to the upper airways which makes breathing easier. This is a bit like blowing up a balloon: a balloon can be more easily blown up if you blow a little bit of air into it first. It is the same with CPAP: the alveoli will not close completely after breathing out, so they will open up more easily with the next breath. CPAP can be given in different ways: with prongs (in the nose) or with a mask. Your baby will alternate between the mask and prongs to help prevent any sores developing on their face. Your baby will also have to wear a hat to keep the system in place properly. The amount of pressure given to your baby will depend on his/her condition.
If your baby cannot breathe by himself, mechanical ventilation is needed. Your baby will be intubated, this is where a tube is inserted into the trachea and the breathing is either supported or taken over by a ventilator. In this case your baby will be transferred to a NICU (Neonatal Intensive Care Unit) if you are not already in one.
Suction Equipment
This is used to remove mucus (and other debris) from your baby’s nose, mouth and throat if it bothers them. The mucus is sucked out through a tube that is inserted into your baby’s nose or mouth by the nurse.
Intravenous drips
Sometimes fluid, nutrients or medicines have to be administered directly into the blood. That can be done in different ways:

Phototherapy lamp
If your baby has jaundice or icterus, it is because the substance bilirubin is increased in the blood (also look up “Bilirubin” in the glossary). This often occurs within the first 2 weeks of life. If the bilirubin level in your baby’s blood is too high (hyperbilirubinemia), it will be treated with UV light. This is called phototherapy and is used to prevent the amount of bilirubin from increasing further. The special UV light from the phototherapy lamp or biliblanket converts the bilirubin into a water form that can leave your baby’s body through the faeces and/or urine.
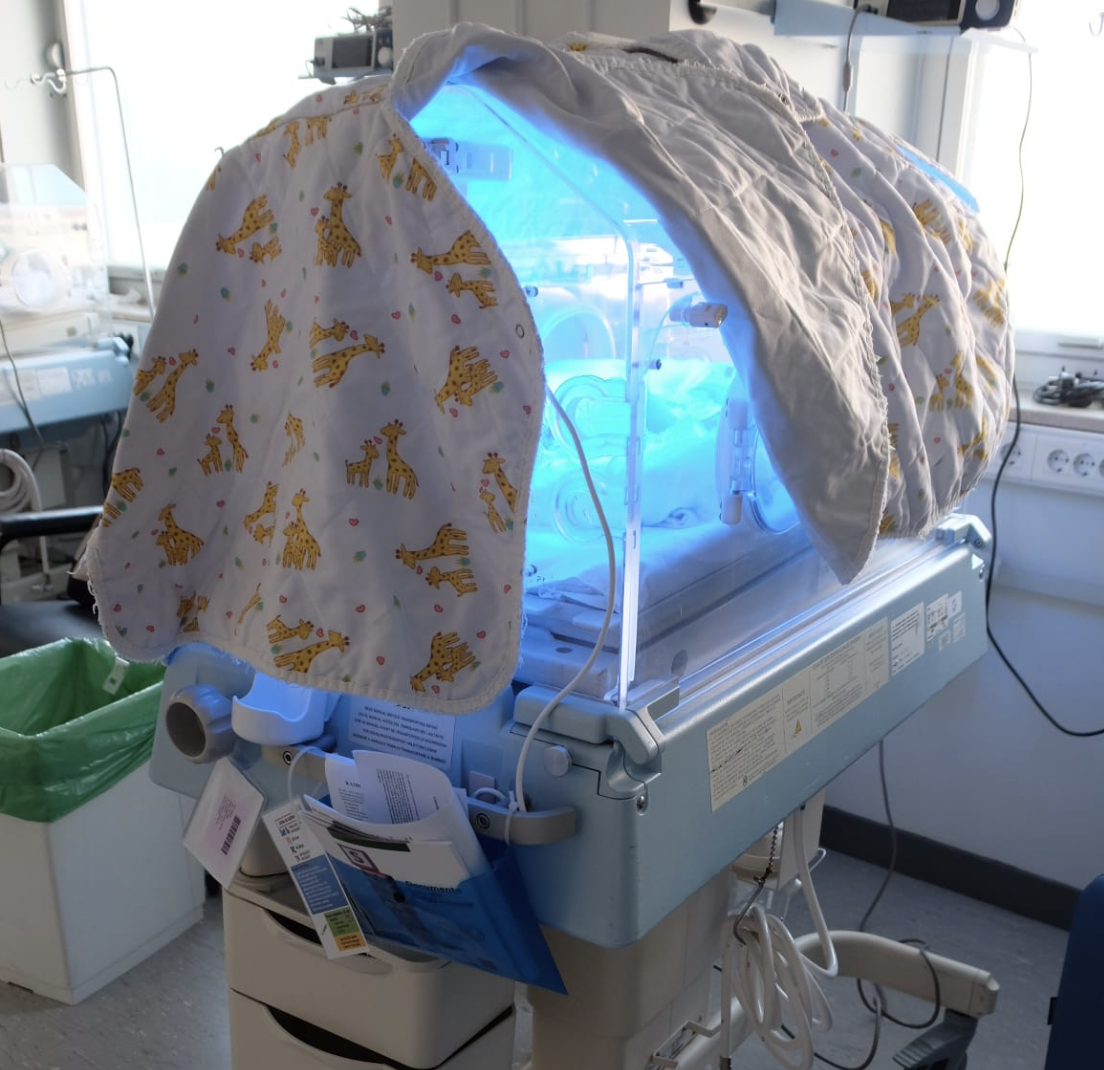
Light therapy can be given with a lamp which releases blue light or LED light above the incubator or heated bed. The lamp can also be put in a mat: the biliblanket or bilisoft. The level of the bilirubin in the blood will determine if your baby needs more than one lamp/use of biliblanket. Your baby will be naked with only a nappy under the lamp (or on the mat) in order to expose as much skin as possible to the light. Sometimes a special extra thin blanket can be used if your baby is restless to make him/her feel safe. The eyes are protected by cloth glasses. If the glasses fall off occasionally , it is not a cause for concern as long as your child has his/her eyes closed..
Every day the amount of bilirubin in the blood is checked to determine the length of time required for phototherapy. Light therapy usually lasts for a few days. When the bilirubin level is low enough, the light therapy will be stopped. After this, blood will be taken again to check that the bilirubin has not increased. It is common for the light therapy to be restarted, but only if the bilirubin level is back to being high again. For more information, see the article, “Jaundice”. Alternatively, a transcutaneous bilirubinometer may be used to check bilirubin levels non-invasively. In order for the treatment to be successful, your baby has to be under the lamp as much as possible. This can mean we ask you to give shorter periods of kangaroo care or cuddles after feeding.
Bladder catheter
Bladder catheterization involves the insertion of a fine tube (catheter) into the bladder through the urethra. Some urinary catheters have a balloon that allows them to be fixed in the bladder to prevent them from moving and coming out. There are several reasons to perform bladder catheterization:
Although this procedure is minimally invasive, complications can occur, such as: infection; trauma; or urine leakage. That is why we will always try to remove the catheter as soon as possible.
PROCEDURE FOR BLADDER CATHETERIZATION
Bladder catheterization is a sterile technique. First, hand hygiene will be carried out, followed by putting on sterile gloves. The area will be cleaned and the probe, coated with anaesthetic lubricant, will be gently inserted. Once its position is verified, the balloon will be filled with sterile water. The catheter will be fixed to the skin of your baby to prevent accidental pulling.
HOW TO CARE FOR YOUR BABY WITH A BLADDER CATHETER
As a parent, it is good to know that the urine collection reservoir should always remain below your baby’s waist to make it easier for urine to come out. Ensure the tube or bag is not bent or crushed. Finally, wash your hands with soap and water before and after handling the bag or tube. When changing the diaper and cleaning the area, avoid contaminating the catheter with faeces. If this happens, wash it with soap and water.
Stoma
A stoma is a therapeutic outlet in the abdominal wall for body waste (e.g. for stool). It is created when the natural outlet does not function (e.g. caused by a congenital malformation or a bowel injury caused by inflammation). The stoma is made by a surgical procedure. We will focus exclusively on the care and management of stomas of the digestive system.
Stoma levels in the digestive system
Stoma care
The stoma should be red, moist and smooth. It may bleed a little if you rub or touch it as it is covered by digestive mucosa which has many blood vessels. . The stoma does not cause pain or discomfort to your baby as there are no nerve endings there. Discomfort may occur if there is abrasion of the skin around the stoma caused by gastrointestinal juices if the stoma bag is not sealed well. The stoma will be washed with water (some neonatal units may also use a neutral soap) with a soft sponge or sterile gauze. The stoma and surrounding skin will be dried with gauze with small touches, without rubbing the mucosa of the stoma.
Stoma care will be directed at three points:
The stoma should always be pink; after surgery it will be swollen, but with the passing of days it can become smaller and change shape. We will monitor the content that comes out, as well as its quantity, colour and texture (yellow, greenish, lumpy, liquid, semi-liquid, etc).
Currently there are two types of collection bags, one-piece and two-piece bags. In both cases, the bag has an opening to empty it. The bag should be emptied each shift to monitor and quantify the amount and content characteristics. The bag will be changed every 1-2 days to avoid contamination.
The skin that surrounds the stoma is very vulnerable. To prevent skin abrasion, it is essential to protect the area around the stoma with barrier products, and adjust the size of the device to the size of the stoma so that there is no leaking.
Treatment of wounds
The skin of the newborn
The skin is the largest organ of the body that acts as a barrier against bacteria. It also acts as a system of communication with the environment. The skin of your baby differs from that of an adult. The skin of a preterm newborn is going to be much thinner and more fragile than that of an adult. Only at 3 weeks of life is the skin of a full-term newborn fully developed. The premature newborn lacks fat because this accumulates in the last trimester of pregnancy. The appearance of the skin is different from that of a term newborn; it is finer, with an intense red colour and with a gelatinous appearance.
All newborns will face the following situations:
Our care, therefore, will be aimed at preventing injuries to the skin, ensuring its integrity, and healing any wounds.
Prevention of wounds
Prevention is the most effective way to avoid injuries to the skin. This involves a detailed assessment of your baby to consider its susceptibility to develop injuries. Part of this care is aimed at correcting and reducing the causes that generate pressure, pulling or friction on the skin.
It is essential to:
Wound care steps

Inhalation medication
Inhalation medication is used to give medication directly into the airway. The devices for aerosols are called inhalers, and those that contain liquid particles, are called nebulizers. Both systems can be used, regardless of which respiratory support your baby is receiving . The most frequently used inhalation medication are bronchodilators (dilators of the airway).
Administration technique
The nurse will always consider whether the moment of administration of a inhaled medication is correct. The inhalation is more effective if your child is calm during. the inhalation.
Administration of medication with an inhaler
Depending on the gestational age and the situation of each baby, the administration will be in the mouth or, more usually, through a nasogastric tube.
Administration technique for oral medication