.1
Neurobehavior
.2
Impact of stress
.3
Pain
.4
Care to provide comfort
.5
Bonding
TAKING PARTIN BABY CARE
The baby´s development
Neurodevelopment
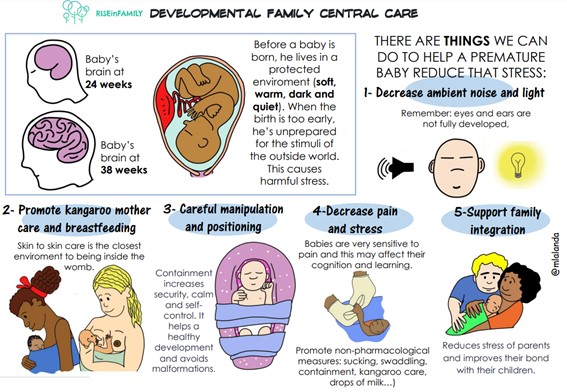
Your baby’s admission to hospital in the department of neonatology represents a sudden change in the surroundings for a newborn (premature) baby to grow and develop. Inside the womb everything is comfortable. In the womb the fetus is curled up and protected by warm liquid that allows the fetus to move smoothly, noises are muffled and there is hardly any light. Outside there is light, noise, gravity, sleep interruptions and repeated manipulations. The brain of a premature or very sick baby is not prepared for such intense stimuli as it is not mature enough to process so much stimulation. The ability of a newborn less than 34 weeks gestation to respond adequately to its environment is poorer, the more immature (lower gestational age) the baby is. Therefore, the medical healthcare professionals and the parents have to try to make an environment that resembles that of the womb to your baby’s growth and development.
To do this, we will focus on different aspects of your baby:
1. Neurobehavior
The term neurobehavior refers to the set of capacities that allow the newborn to interact with its environment, that is, to communicate with us. You, with the help and advice of the neonatal team, will be able to learn to know your baby, recognize his/her needs by observing his/her behavior, and act in the most appropriate way so that your baby learns to control himself/herself and calm down, or what we sometimes call, self-regulation. This will have a positive impact on his/her development. We will also help you adapt environmental factors at all times, taking into account the gestational age and the clinical situation.
We must not forget that each newborn is unique and will have their own needs, hence the importance of participating in the care of your baby.
Newborns exhibit several different patterns of behavior that we call “states”. You can see the characteristics of how they are awake, how they go from being awake to asleep, how they experience stimuli, etc., This helps you understand what your baby needs.
There are differences between the states of term and preterm infants. In general, in a full-term newborn we can easily identify how they go from being asleep to being awake, they have better tolerance to environmental stimuli and they have the capacity for self-regulation. In contrast, in premature infants, sleep periods are longer, they are awake for less time, they are more affected by external stimuli and they have little self-regulation capacity. This changes as they mature.
How does your baby react to the environment?
To know if your baby is calm or not, we observe his/her bodily reactions to the environment that surrounds him/her. These behaviors can be of two types:
BALANCE BEHAVIORS
The baby is calm (organized) if he/she has:
WITHDRAWAL BEHAVIORS
the baby is not calm (disorganized) if he/she has:
We always have to observe your baby thoroughly. An isolated behavior does not accurately define how your baby is responding to the environment.
2. Impact of stress
The stress response in the developing baby is not always negative. In fact, there is also positive stress. For example, brief increases in heart rate or elevation of stress-regulating hormones that help prepare the body to react appropriately to stress-causing agents.
We refer to tolerable stress when the response to it can potentially induce changes in the developing brain but limiting it to specified periods of time to allow recovery so that damage can be avoided to the structure and function of the brain.
Finally, we speak of toxic stress when it provokes a strong, frequent or prolonged bodily response. This type of stress can have an impact on brain architecture.
If we know and identify the signs that show toxic stress in your baby, we can help him/her recover to a state of balance for his/her best development.
3. Pain
How is pain in newborns different compared to children and adults?
Nowadays we know that newborn babies, as well as premature babies, already have a well-developed ability to feel pain. Recognizing and managing the pain is very important for the baby’s health. In addition, studies have shown that pain management in newborn babies can contribute to a better long term outcome]. As a result of this new knowledge much progress has been made in the treatment of pain in newly born babies. Pain in newly born babies differs from pain experienced by children and adults. Reasons for this are:
Unfortunately, not all pain can be avoided, especially in the first few weeks of hospitalisation when many (possibly) painful activities are often necessary. Among which are, for example, inserting a drip or taking blood samples.Despite the painful nature of these activities, it is important to recognize the pain, and as a parent you can really help your baby with this. To recognize the pain and comfort your baby, the nurse will help you.
Recognizing pain:
Recognizing pain to some extent depends on your baby’s behaviour and health. Similarly, the surroundings (such as light and sound) can influence the recognition of pain. Nurses often use a pain score to rate the pain they see in your baby. There are various pain scores, such as the Comfort score. With the Comfort score the nurse can estimate the pain by looking at a number of the baby’s characteristics for two minutes: alertness, agitation, breathing, blood pressure, heart rate, crying, movements, muscle tension and facial tension.

Because your baby cannot talk yet, your child uses his face, arms, legs, breathing and vocal sounds to express himself. When a newly born feels pain, you can see the following characteristics:
The heart rate may also increase and the oxygen level in the blood may decrease. Babies who have long-term pain, however, move little, react little to stimuli and are quiet. These are also signs of pain.
Pain treatment: Parents are important allies in pain management. By involving you as a parent, pain management can be given in an appropriate manner. You can help by comforting your baby in one of the following ways. You can ease the pain by letting your baby suck on a pacifier, rocking, talking to your baby or by putting a hand on his head and/or bottom and rocking gently. Besides comfort given by you as a parent, we can give your baby medication to manage the pain. If your baby’s blood has to be taken or an intravenous catheter has to be placed, we will put some sucrose in his mouth beforehand. This is a sugar dilution that decreases the pain and stress. The sucrose is put in the mouth and has no side effects. If your baby is in pain for a longer time, we can give paracetamol. This can be given orally, by an intravenous drip or by a suppository. Strong pain medication is, for instance, morphine or fentanyl, that will be prescribed by your doctor if needed.
Also refer to the article “Comforting your child”.
4. Care to provide comfort
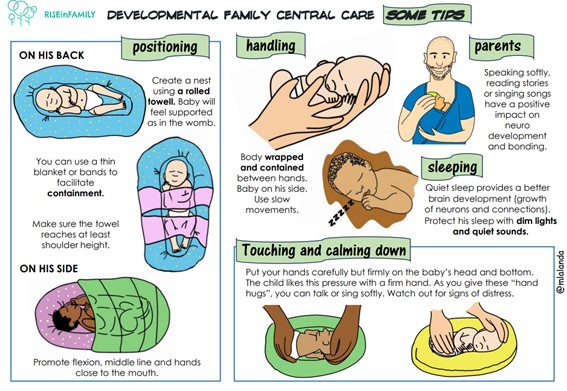
POSITIONING
Containment is the way of “caressing” that your baby likes the most, especially when he/she is very small or premature. Their nerve endings are not prepared for a lot stimulation, and the caresses that we are used to are excessive for them. It consists of supporting your hands, having warmed them up beforehand, on his/her head and legs, on his/her head and gently grasping his/her arms, or on his/her arms and legs, facilitating flexion.
The objective of positioning is for your baby to maintain a physiological position, to favor musculoskeletal development and improve its physiological functions, as well as to reduce the complications derived from incorrect posture. Postural changes should be applied to all newborns, but in the case of the premature newborn or if your baby is sedated, special attention should be paid. This is because these patients lack the ability to maintain correct posture.


NEST
Nests are commercial or self-made devices, through the use of rolled towels or sheets, which form an oval that imitates the maternal uterus. The nests must have the appropriate height, which promotes the flexion of the limbs on the trunk and their orientation towards the midline. Your baby must find limits in the nest, but at the same time, it must be able to move. We will know that the size of the nest is not adequate (small) when the device does not contain your baby’s shoulders in a supine position (face up), or if the device cannot maintain the correct posture of the newborn, favoring flexion and midline orientation. The nest is a fundamental element to increase the baby’s perception of support and security, and promotes self-regulation behaviors. As your baby becomes more competent, he will need more space and be able to move more freely.
Different postures

HANDLING
The rest of your baby is essential for his/her development. Whenever possible, your baby’s sleep and comfortable rest will be respected, avoiding interruptions. The lower the postmenstrual age of your baby, the greater the difficulty in identifying if he/she is asleep or awake, and if he/she is ready for us to do all the necessary care. That is why it is important to know the different ways you have to communicate with us. Until 32 weeks of postmenstrual age they do not begin to awaken spontaneously. When babies reach the maturational age of 38-40 weeks, in addition to waking up on their own, they are able to maintain longer cycles of deep sleep. Wake-sleep cycles should be encouraged. In premature babies, low-intensity light-dark cycles are recommended, which remind the light differences of day and night, to favor their growth and development. A 12-hour light cycle can be provided from 32-34 weeks postmenstrual age, preferably natural light, avoiding direct exposure to the baby’s face; and a 12 hour dark cycle. This will always be done individually and progressively.


REST
The rest of your baby is essential for his/her development. Whenever possible, your baby’s sleep and comfortable rest will be respected, avoiding interruptions. The lower the postmenstrual age of your baby, the greater the difficulty in identifying if he/she is asleep or awake, and if he/she is ready for us to do all the necessary care. That is why it is important to know the different ways you have to communicate with us. Until 32 weeks of postmenstrual age they do not begin to awaken spontaneously. When babies reach the maturational age of 38-40 weeks, in addition to waking up on their own, they are able to maintain longer cycles of deep sleep. Wake-sleep cycles should be encouraged. In premature babies, low-intensity light-dark cycles are recommended, which remind the light differences of day and night, to favor their growth and development. A 12-hour light cycle can be provided from 32-34 weeks postmenstrual age, preferably natural light, avoiding direct exposure to the baby’s face; and a 12 hour dark cycle. This will always be done individually and progressively.
5. Bonding
During your pregnancy you probably already talked to your child, you stroked your tummy. More or less unconsciously you were already creating a bond with your child. While your child is in hospital, he has to deal with many people around him. That makes good bonding more difficult. Nevertheless, in the department of neonatology attention is already given to the bonding between you and your child. Physical contact is stimulated and the signs your baby shows are explained to you, so that you can react properly to them. By reacting in the same way every time to your baby’s signs, you become predictable for your baby. This is incredibly important, now and for the rest of his life. In the first few weeks with your help, your baby will take an important step in building self-confidence (‘I can show what I need) and in confidence in his parents (‘They understand me and they look after me’). Making contact with your child is very important for growth and development. The short moments of contact in the beginning teach him to recognize you as the person he really belongs to. Your baby will for instance recognize your smell and your voice. Making this contact is also important for you to start bonding with your child. You get to know and already understand each other. For example, many parents quickly see which position their child likes, although your child is not yet able to move in such a direct way in response to touch. Very premature children often cry without sound, but you can see tension or sadness on their faces when they are uncomfortable or in pain. Then you can comfort your child with your voice, a touch or skin-to-skin contact. For instance, put your warm hand on his bottom, tummy or head or against his feet. At the same time, talk in a soft voice or sing a song. This will quieten your child. Try to feel what your child can handle and what he needs. By watching him closely you will learn to recognize signs in his behaviour. In this way you can adapt your own reactions. We will help you with this in the department.
When you have found out what is comforting, you can also support your child during medical procedures that are unpleasant or painful for him. Also refer to the article “Comforting your child”.
Babies of 37 to 42 weeks (full term)

Making eye contact
Children who are ill, premature or SGA make much less eye contact compared to full-term and healthy children, especially in the first few weeks. They also move less and cry softly. Do not worry, that is normal. You can try, however, to make eye contact yourself, even through the incubator. Preferably dim the light, as your child tends to squeeze his eyes shut in bright light. The development of eye contact is important in creating a strong parent-child bond. Having patience is part of it; let your child set the pace. If your child adverts or shuts his eyes, he is giving himself a rest to process the stimuli.
There is also a difference between watching and seeing. In the beginning your child looks at you, but he also turns to the light. Only later does your baby start to perceive more consciously and he learns to really see.

Infant colics/tummy massage
Stomach cramps often occur in babies. On average, the peak of the stomach cramps is at the age of 6 weeks and the stomach cramps are gone again at 12-16 weeks.
The symptoms of stomach cramps can differ per child, but most babies cry, strain, have their legs tucked up and suffer from flatulence. As a parent this can make you feel uncomfortable and powerless. The exact cause of the stomach cramps is not known. Stomach cramps are probably caused by various factors at the same time. Various possible causes have been researched in studies:
No effective treatment with medicines is known, but as a parent you can make sure that your baby rests and relaxes when he/she has infant colics. Tummy massage is one of the activities a parent can do to relax your baby. By giving a tummy massage you ensure relaxation, rest and a better digestion of the food.
Step-by-step plan for tummy massage:

Other things you can do in the event of stomach cramps are: putting a warm hand on your child’s tummy, skin-to-skin care, carrying your child in a sling or swaddling your child.
Physiotherapy
Children who are born premature, SGA or ill really need their parents to adapt their surroundings to avoid overstimulation and help them to regulate their reactions to them. A paediatric physiotherapist or occupational therapist can help you with that. Besides that, a paediatric physiotherapist can give you solid advice on how to challenge your child in the next phase of his development. Paediatric physiotherapy is included in the basic health insurance policy.
Pain and comfort
Positioning and handling