TAKING PART IN BABY CARE
Premature birth
Prematurity: in general
A baby that is born too early is called premature. That is to say, when your baby is born before the 37th week of pregnancy, we speak of a prematurely born baby. The younger the baby is at birth, the more likely it is that the baby will need support in different ways.
Possible causes of a premature birth are:
Sometimes the cause is not clear.
Characteristics of a premature baby

Special care for the premature baby
How premature your baby is, largely determines what kind of special care your baby needs. We are extra alert to the following points:
Because of the lack of subcutaneous fat, your baby is insufficiently capable of keeping him/herself at the right temperature and therefore will be placed in an incubator or heated bed. Depending on your baby’s birth weight, gestational age and temperature, a bed preheated with hot water bottles is sometimes already sufficient.Besides that Kangaroo Care can assist to maintain the best temperature for your baby.
With a monitor we can, if medically needed, monitor the amount of oxygen in the blood, heartbeat and breathing. Small stickers are placed on your baby’s chest and a little cuff/sensor around an arm or leg. Premature babies younger than 34-35 weeks are always connected to a monitor. Breathing problems may occur due to the immaturity of the lungs. Pauses in breathing (apnoea) and a drop in the heart rate (bradycardia) may occur. These can right themselves spontaneously. Sometimes they can occur because the airway is obstructed and/or misplaced. When we observe such events we have to check the positioning and if it’s necessary, correct it. In addition to observing the trend of the breathing line on the monitor. The breathing of your baby is irregular and sometimes periods of superficial and/or periodic breaths are observed (alternating superficial breaths with deeper breaths). Stimulation is not always necessary. If necessary, stimulation has to be at first gentle, as a light massage on the back and if your baby does not respond a bit stronger. If these events persist or if your baby often has to be stimulated, breathing support can be offered and perhaps medication (caffeine) will be necessary to stimulate breathing.
If your delivery started before 34 weeks of pregnancy, you probably had injections for iproving your baby’s lung maturity (corticosteroids). Depending on your baby’s age and clinical condition, it is possible that we will support him in breathing.
Because your baby has small energy reserves, keeping up the blood sugar level is often difficult for him/her. For this reason, blood checks are necessary on a regular basis. This is done by pricking the heel. In the event of the blood sugars being too low, extra nutrition will be given or a glucose-intravenous drip may be necessary.
Due to the immaturity of the liver, your baby can turn yellow for up to a few days after birth. Bilirubin (a waste product) is processed and secreted by the body. High levels of bilirubin can result in yellowing of the skin known as jaundice. Blood will be taken in order to determine the bilirubin level. If the level is too high, then your baby will start phototherapy. During phototherapy, your baby will be placed under one or more blue or LED lamps. The phototherapy can take a few days. The bilirubin level will be checked daily. Also look at the article “Jaundice”.
From 33-34 weeks the sucking, swallow and breathing coordination starts, enabling your baby drink by himself. If your baby is younger than this, then your baby will get a gastric tube through which the nutrition can be given. A baby of 32-33 weeks will often also get an intravenous drip to receive extra fluids and nutrients. From about 35-36 weeks your baby can often drink mostly by himself. As your baby gets older, he will drink better and the gastric tube will not be necessary anymore. In some hospitals you can take your baby home with tube feeding if you have had good guidance on using it.
If your baby is born prematurely and you want to start breastfeeding, it is good to introduce your baby to breastfeeding at an early stage. It is important that he gains positive experience on the breast and often gets the chance to practise. As long as your baby cannot really drink from the breast, it is important to stimulate the milk production by expressing. The expressed milk can be given by the gastric tube.
Your baby’s weight will be checked daily, unless otherwise agreed. The amount of fluid and/or feeding is decided according to the weight. The head circumference and length will be measured once a week.
When your child is asleep, try not to wake him. When your baby is slowly waking up, put your hands on him and speak softly. Avoid noise and light in your baby’s bedroom and make sure there are periods of rest so that your baby can save energy. Your baby can start learning to sleep on his back. This is the sleeping position that is recommended for at home. While your baby is on the monitor, he/she can be positioned on his tummy too. The tummy position is only done on the advice of the doctor or nurse to support the breathing better.
Good positioning and confinement around your baby’s body will make sure that your baby is comfortable and it will help him grow. For this a snuggle, bumper/towel roll and frog are used. You can read more about this in the article “Developmental care”. When caring for your baby, you can put your hands around him to offer comfort.
We encourage you to be involved in your baby’s care as much as possible. Naturally we will help you, such as by taking his temperature, changing a nappy and giving a bath. With improving your skills, you will be able to provide your baby more specialized care, together with your nurse. Your presence is important for your baby’s well-being and development. Also look at the article “Family Integrated Care (FICare)” and “Caring together”.
All babies (especially premature babies) have the need to suck. Sucking on a pacifier during tube feeding helps to make the association between sucking and a full tummy. It also improves the oral muscle tension and coordination.If the mother is present and wants to breastfeed you can also use the nipple at an empty breast to improve the breastfeeding.
Learning how to drink and premature birth
Premature children drink differently to children born full-term. A child needs to be able to alternate between sucking, swallowing and breathing in order to be able to drink by himself. Often there is still less rhythm in this sucking-swallowing-breathing pattern, because it is not yet automatic. This means that your child needs extra time to suck and swallow, and longer breathing pauses to catch his breath. In addition to being born prematurely, there can be other causes why your child cannot drink enough by himself, for instance, because of heart or lung problems or neurological problems.
From about 33-34 weeks of pregnancy, your child will be offered the first milk orally. Most children have enough coordination to suck, swallow and breath around 35-37 weeks. This can vary according to your child’s health and the OSMO and Kangaroo Care that is provided.
Also look for more information in the article “Learning how to drink”, “OSMO” and the other articles in the chapter “Feeding Your Baby”.
Donor milk
Donor milk is expressed breastmilk that a mother donates to another child. Also there is the Human Milk Network, where recipient mothers and donor mothers are brought into contact with each other. All applications to the Human Milk Network have to be supported by a health care professional, such as a GP, midwife, paediatrician or child health specialist.
Only donor mothers who do not smoke and who do not use medication, alcohol or drugs are eligible to donate breast milk. There is also a screening for infectious diseases, such as HIV, Hepatitis B and C and syphilis. The Dutch Human Milk Bank also screens for CMV, because this virus presents a possible extra risk to prematurely born children. Expressing, pasteurizing, keeping and transporting donor milk is done according to the regulations.
Feedings and supplements
A premature and/or SGA baby needs a different combination of nutrients than a term baby. The best food for your child is your own or donated breast milk. However, protein, energy and minerals, such as calcium, may not be in sufficient amounts in breastmilk.It may therefore be necessary to add extra supplements to the feeding.
BMF
If your baby gets expressed breastmilk, BMF is often added. BMF stands for Breast Milk Fortifier, which is a powder that can be mixed with breastmilk. BMF contains extra calories, carbohydrates, proteins, vitamins and minerals.
LIQUIGEN
Liquigen can be added to give more calories to your baby’s feed. Liquigen is rich in energy and can be given if, despite previous supplements, there still is not enough growth.
CALOGEN
Calogen can be added to give more calories to the feed. This also stimulates your baby’s growth.
PROTEIN FORTIFIER
If your baby shows insufficient growth, your doctor can choose to add Protein fortifier to enrich the feed. This is a powder that can be mixed with milk. It contains extra proteins that are necessary for sufficient growth.
SPECIAL FORMULA FEEDING FOOR PREMATURE BABIES
if you are not capable of giving breastmilk or choose not to, formula feeding for premature babies can be given. These infant formulas are developed especially for premature and SGA babies. These formulas are enriched with nutrients like vitamins and minerals and extra energy.
Correcting the age for prematurity
When looking at a premature (<37 weeks of pregnancy) baby’s development, one term always turns up: the corrected age. The corrected age is the age your baby would have been if he had been born on the due date (40 weeks). The age since birth is also called the calendar age. You can calculate the corrected age by subtracting the number of weeks your baby was prematurely born from the calendar age.
For instance: your baby is now 12 weeks old (calendar age and was born 4 weeks too early). The corrected age is then 8 weeks (12 weeks – 4 weeks), in other words, 2 months old. As far as development is concerned, your baby may be compared to other 2 month old babies.
People around you do not always know what a corrected age is. Do not become anxious if somebody asks you why your baby does not smile yet (“He is already 3 months old, isn’t he?”). You can then explain that he is actually only 2 (corrected) months old.
In principle, the corrected age is used up to the age of 2 years.
Medication
While in hospital, your baby may have different medicines. Here is a short explanation about the medicines most often used:

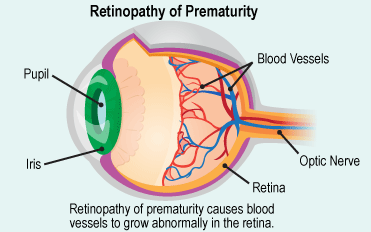
Retinopathy of prematurity (ROP)
In some extreme premature babies, the blood vessels in the retina of the eye develop differently or are not fully developed. When the wrong blood vessels and scar tissue grow on the retina, we call this a retinal abnormality. If the vessels grow in a disorganized way it is called Retinopathy of Prematurity (ROP). ROP tests will be done in the following premature babies:
The eye examination will take place several times until the ophthalmologist sees that the vessels on the retina have grown properly. In serious cases it may be necessary to start treatment because the retina may tear (this is very rare). This treatment is done in the NICU where they cauterize the abnormal blood vessels using laser treatment or local injection of specific compounds to stop vascular proliferation.
The parent or nurse can help and comfort the baby during the examination. It is possible that as a parent you do not like the examination. The ophthalmologist actually has to keep your baby’s eye open with a speculum to be able to have a good look at the retina. The eye examination itself takes less than 5 minutes. The pupils are dilated as a result of the eye drops and this can last a while. Therefore, make sure that your baby does not get any bright light in his/her eyes after the examination.
Bronchopulmonary dysplasia (BPD)
Bronchopulmonary dysplasia (BPD) is a chronic lung condition that is characterized by long-term breathing problems. This problem is mainly seen in premature babies (<30 weeks) who need breathing support (like invasive ventilation or CPAP). Some BPD patients have only been on the CPAP. We speak of BPD if a baby has reached the age of 36 weeks after conception and still needs extra oxygen or breathing support. When your baby is around 36 weeks, it might be necessary to determine the degree of BPD with a test: the oxygen reduction test. Whether or not this test is necessary depends on the support your baby has at that moment in time. The degree of BPD is divided into mild, moderate/serious and serious BPD.

Exactly how BPD arises is still unclear. It is thought that the ventilation/CPAP/oxygen/infection has an effect on the as yet not fully developed lungs. There is damage to the alveoli and pulmonary vessels. This causes scarring and changes the structure of the alveoli and pulmonary vessels. Because the structure changes, fluid can leak into the lungs. As a result, the baby has to work harder to breathe and sometimes, depending on the severity, needs extra oxygen.
Using the current techniques, we can often prevent BPD and luckily also treat it better. Depending on the seriousness of the BPD, the treatment consists of several components. Fluid overload has to be avoided, therefore diuretics can be prescribed as well as fluid restriction. Your baby may only drink up to a maximum amount to ensure that he/she does not retain too much fluid. It is usually possible to stop the use of medicines before discharge. Occasionally it is necessary to go home with oxygen. Furthermore, it is of importance that these children keep on growingso that the lungs can recover. Therefore, sometimes the feed is enriched with extra nutrients (also look at the article “Feedings and supplements”). New alveoli are produced up to the age of six.
Because breathing in babies with BPD takes extra energy, it may be that BPD babies do not drink well. Occasionally a baby will go home with tube feeding. Babies with BPD suffer from respiratory infections more often and are re-admitted to hospital more often. This is predominantly in the first year of life. They take antibiotics more often and sometimes receive medicine for their airways. If your baby has serious BPD, in addition to check-ups by the paediatrician/neonatologist, your baby will also possibly be checked by the paediatric pulmonologist and the paediatric cardiologist at a university hospital.
RSV vaccination
In addition to the vaccinations on the national vaccination programme (see also article “Vaccinations”), an extra vaccination against the Respiratory Syncytia virusl (RSV) is available for premature or ill children. This is advised for the following group of children:

Symptoms of the RS virus
Usually this virus only causes a nose cold in adults and children. But in younger children, the RS virus can also affect the lower airways, which may cause the child to have breathing problems, apnea and feeding problems and a stay in hospital may be needed. Every winter you hear about this in the media. In the Netherlands, the RS season usually lasts from October to April.
Preventing infection:
To help prevent infection by the RSV you can do the following:
The vaccine against the RSV:
In this passive vaccination (prophylaxis), antibodies against the RSV are given by an injection in the upper leg. A passive vaccine works differently from vaccinations with a weakened virus or bacteria. In addition, the child still has to produce the antibodies him/herself. The advantage of the vaccination against the RSV is that your child will not become ill from it. Your child will therefore not need to be hospitalized for monitoring. A disadvantage is that the antibodies break down quickly, so that your child will need to have the injection every month during the RSV season. The vaccination does not provide full protection: your child can still become ill from the RSV, but after vaccination the infection is usually less serious and a stay in hospital is rarely necessary.
Discuss whether you want to have the vaccination with the paediatrician.